By Drake Bennett and Michelle Fay Cortez
As undergraduates returned to the University of Arizona for the fall semester, many of the new precautions were hard to miss. Plexiglass dividers were affixed in front of lecterns and between lab benches. Giant tents were set up so students arriving early for a class could wait outdoors, sheltered from the punishing sun. Roving teams of student “health ambassadors” tooled around in golf carts, handing out masks and politely chiding their peers for standing less than 6 feet apart.
But the first thing students had to do was visit one of the university gyms for a rapid SARS-CoV-2 test. The results took an hour. Negative, and you could move into your residence hall right away. Positive, and you were sent to a special isolation dorm, where you spent the next 10 days taking classes online.
Many of these safety measures emerged from discussions headed by Richard Carmona, a former U.S. surgeon general who’s a professor of public health at the university. Carmona’s medical career stretches back to the Vietnam War, where he served as a special forces medic after dropping out of high school. Over the years he’s developed an expertise in emergency preparedness and disaster response. As news of the novel coronavirus began making its way out of China last winter, the university’s president asked Carmona to form a working group and propose ways to keep the institution functioning during a pandemic. “The question was, what were the metrics we’re going to look at and how are we going to be able to make a reasonable determination that this is somewhat safe?” Carmona says. “We didn’t have a playbook for this. Nobody had a playbook.”
In early spring the team reached out to Ian Pepper, an environmental microbiologist on the faculty who had experience with wastewater testing. “It used to be called sewage surveillance,” says Pepper. “Now the preferred term seems to be wastewater-based epidemiology.” The technique traditionally has been used in population-level studies of illegal drug use or viral infections. Carmona’s team, however, wanted to go upstream from the treatment plant to determine not just if the coronavirus was on campus, but where. The sampling would provide an early warning system—people ill with Covid-19 can start shedding the virus in their stool as many as seven days before showing symptoms. “That gives you seven precious days for intervention,” Pepper says.
Over the summer, Carmona pored over university blueprints with the facilities department, tracing decades-old sewage pipes back to the dorms they drain, while Pepper worked on filtering samples and identifying trace amounts of the virus. By the time students returned in August, the program was in place. Each morning at 8:30—an hour chosen to give residents a chance to visit the bathroom—a faculty engineer working with an undergrad assistant would make the rounds, at each stop prying off a manhole cover and lowering an open Nalgene water bottle at the end of a long aluminum pole into the river of waste below. The pair would place the samples in a cooler and drive them back to the lab, where Pepper’s crew would turn around the results by the afternoon.
On Tuesday, Aug. 25, a week and a half after students started to return, Pepper got his first positive, from the pipe leaving a dorm called Likins Hall. The next day, all 311 Likins residents took Covid tests. Two students, both without symptoms, came back positive and were relocated to the isolation dorm. Thanks to the head start, no other residents would contract the virus.
Since then, the university has stemmed outbreaks in at least eight other dorms using the same method. Pepper is scaling up his lab, training more teams of samplers, and expanding the effort to off-campus apartments and Greek houses. He’s fielding requests from around the world for help setting up similar programs. Carmona, for his part, is careful not to get ahead of himself. “It’s a tool that’s just evolving,” he says, “but we see value.”
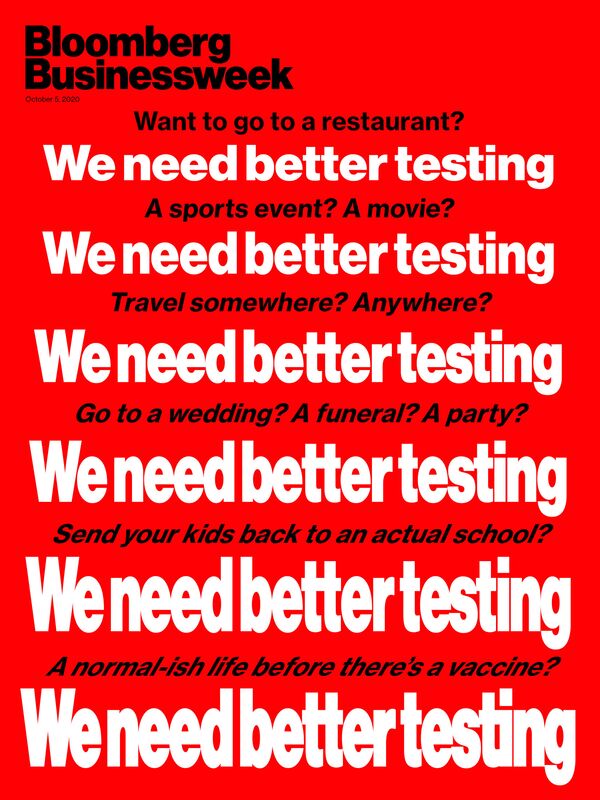
Ever since the novel coronavirus began circulating in the U.S., the country’s response has been crippled by a failure to see the spread in anything close to real time. Half a year after the first wave of U.S. lockdowns, with more than 200,000 Americans dead from Covid, we’re still playing catch-up. The Trump administration’s botched rollout of its first tests, and the supply chain shortages that followed, helped the disease spread unchecked. Today, processing bottlenecks still render many test results worthless by the time people get them. This blindness has left public-health officials only the crudest measures of containment, such as broad social distancing mandates and lockdowns. It’s turned the loosening of restrictions on restaurants, sports, offices, gyms, and schools into terrifying leaps of faith. And it has surely killed people.
“The testing we are doing today is mostly just keeping score for the virus,” says William Hanage, an epidemiology professor at Harvard. Even that grim framing gives the U.S. system too much credit. The Centers for Disease Control and Prevention’s sampling of Americans with SARS-CoV-2 antibodies shows that the true number of infections is as many as seven times higher than the official count.
Over time, though, the problem of testing has attracted new focus, new thinking, and new money. Experimental viral screening technologies have taken big steps forward, and researchers have found ways to retool existing procedures. Some of that work isn’t likely to pay off in time to change the course of the pandemic, but some of it already has. And the outbreak’s global scale has spurred epidemiologists and policymakers to seek better answers to fundamental questions about the management of a modern plague: not only how to test but whom to test, and why.
New Daily Covid-19 Cases in the U.S.
Seven-day rolling average
Data: The Covid Tracking Project
Those debates are particularly vital now. The number of new U.S. Covid cases, which peaked this summer before dropping significantly, is climbing again—the CDC’s seven-day moving average rose from 34,371 on Sept. 12 to 44,307 on Sept. 26. Colder weather and classroom reopenings threaten an explosion of cases at a time when the public has tired of social distancing’s heavy costs. And we’re still, at the earliest, months away from a working, widely available vaccine.
Until then, testing can help close the gap between normalcy and where we are. If Americans want to safely send kids to school, eat in a cafe, go to a basketball game, or get on a plane, the U.S. needs to test a lot more people a lot faster. Faster, cheaper testing may not flag every new case of Covid, but that shouldn’t mean settling for the current level of blindness, with its torturous drip of preventable deaths. Even world-class testing won’t rid us of the virus, but it can allow us to live our lives in the meanwhile.
Well before this year, the U.S. had ample warning about the health-care system’s vulnerability to a pandemic. An industry long kept as lean as possible lacked the personnel and hospital beds needed to respond to a national crisis, let alone the protective gear and ventilators the coronavirus requires. Testing was the one thing the U.S. had supposedly handled. The CDC’s early warning system for epidemics, based on reports from medical professionals all over the country, was designed to spot new diseases in time to head off bigger problems. And the technology to create tests for new viral diseases is so straightforward that it can generally be done in a few days.
When the time came, though, the apparatus worked against itself. After its Chinese counterparts published SARS-CoV-2’s genetic sequence on Jan. 11, the CDC did indeed create its own test in a matter of days—but because of regulatory requirements and limited access to the relevant viral samples, the agency’s Atlanta headquarters was the only place it could be done. In early February, the CDC produced tests that state labs around the country could use, but they were faulty and returned inconclusive results. Public and private clinical labs rushed to fill the void, only to be stymied by the Food and Drug Administration, which demanded extensive data and a regulatory submission before authorizing alternatives.
By early March, the U.S. was struggling to run 1,000 tests a day, while South Korea, which confirmed its first case the same day the U.S. did, was running 10,000. By the end of that month, lab giants Abbott Labs, Hologic, LabCorp, Quest Diagnostics, and Roche had rolled out U.S. tests of their own. But at $100 to $150 apiece, they were expensive, and labs were short on technicians trained to run them. Long, complex supply chains led to further shortages, from the swabs needed to gather nasopharyngeal samples to the reagents used to process the tests.
The tests in use at the time were molecular diagnostics known as polymerase chain reaction tests. Performed by medical professionals and processed in specialized labs, PCR tests identify segments of a virus’s genetic material in secretions swabbed from the back of a patient’s throat or nose. The process starts with enzymes being added to the sample, which is then repeatedly heated and cooled to create billions of copies of the viral genome. Special “probe” molecules bind to the copied genetic material, releasing fluorescing nanoparticles whose glow signals the virus’s presence.
Used in everything from food safety to DNA profiling, PCR tests take several hours and are extremely sensitive; if the virus is present in a sample, even in infinitesimal amounts, PCR will find it. To public health officials in the early days of the pandemic, reliability seemed like the most important quality. But the hospitals, doctors’ offices, and pop-up testing facilities where PCR tests are given often don’t have the equipment to process the results on-site—the thermocycler that incubates the samples costs at least $100,000—so the swabs are usually sent out. That’s resulted in massive backlogs and severely limited the tests’ usefulness.
There are alternatives. One, a lateral-flow test, is a disposable strip of cellulose or woven fiber—picture a home pregnancy test. Instead of looking for viral DNA or RNA, it identifies proteins called antigens that protrude from the virus capsule. It exploits the lock-and-key relationship between those molecules and the antibodies the human immune system makes to identify them.
Lateral-flow tests can be done on nasal swabs, but some are in development to work with saliva. The sample is deposited at one end, doused with liquid, and then spreads through the fiber by capillary action, like a spill infusing a sponge. As it advances, the solution flows over antibodies embedded in the fiber with nanoparticles of gold or dye grafted onto them as tags. If the virus is present in the sample, the antibodies latch on and are carried along until the virus-antibody pair encounters a second set of antibodies anchored in a line. Those, too, grab onto the target viruses, activating the tags on the antibodies that hitched a ride earlier. As more virus-rich liquid reaches the line, the tags, like millions of microscopic pixels, form the telltale stripe of a positive result. The whole process can take as little as 15 minutes.
OraSure Technologies Inc. has long sold lateral-flow tests for hepatitis C and HIV. In 2017 it created the only FDA-approved Ebola antigen test. The company is based in Bethlehem, Pa., but sells many of its fast, cheap, over-the-counter diagnostics in sub-Saharan African nations that lack the medical infrastructure for PCR testing. At the beginning of this year, with the U.S. struggling to create reliable tests and its most advanced labs overwhelmed, Chief Executive Officer Stephen Tang saw the parallels.
“We have to repatriate our experience from low- and middle-income countries,” he says. “You have a test that is rapid, that you can take by yourself, that doesn’t require an instrument to read or a medical professional to administer. What we have learned from experience is that people will test themselves more frequently in the privacy of their own homes.” Tang plans to build on the company’s HIV test platform to bring an at-home Covid test to market before the end of the year. While the HIV test costs $40 to $50 in a U.S. pharmacy, the company promises its coronavirus test will be cheaper.
Other strip-test makers have also prioritized the pandemic. E25Bio, a startup born in an MIT lab two years ago, has temporarily shifted its focus from epidemic fever viruses such as dengue and Zika. “With Covid, there have been maybe 50 million infections worldwide,” says CEO Bobby Brooke Herrera. “Dengue causes 400 million every single year.” Like Tang, Herrera has been trying to apply lessons from countries with threadbare public-health systems to those like the U.S. He’s in discussions with U.S. regulators to authorize a coronavirus strip test made to be processed in a lab. Once it reaches the market, he says, a home version will be next.
Established testing companies are already bringing lateral-flow tests to market. On Aug. 26, Abbott Laboratories announced that the FDA had awarded it an emergency use authorization for BinaxNOW, a 15-minute disposable antigen test priced at $5. A so-called point-of-care test, it must be given by a health professional. But since it requires no lab equipment, an unlimited number can be conducted and processed at any given time. Abbott is already producing 50 million of them a month.
A test’s accuracy is a matter of sensitivity (how often it correctly spots a disease) and specificity (how often it correctly rules the disease out). A test with low sensitivity will miss lots of cases; a test with low specificity will mistakenly tell people they have a disease when they don’t. Lateral-flow tests are neither as sensitive nor as specific as PCR tests. They’re more likely to miss an infection during the incubation period, as the invader has just started replicating, or weeks in, when the body’s immune response has managed to eliminate many of the virus particles.
For more information go to: www.bloomberg.com